.
Private Childbirth & Breastfeeding Education
Providing private in-person and virtual Childbirth & Breastfeeding Classes for a positive birth experience. Click Private Class Enquiry for more information.
Ever heard a woman tell this story? Once upon a time the lady’s labor began with a long Pitocin (UK-Syntocinon) induced labor, an epidural for pain and either a long pushing stage or a C-Section? The mother felt an overwhelming joy when the baby was born and relief that the labor was over. But within minutes she was introduced to the new and real demands of parenting which start with breastfeeding a baby every 2-3 hours day and night. Then, just when she thought the hard part was over and she was discharged home, her baby started cluster feeding, became jaundiced and lost >8% of his/her bodyweight by the pediatric visit on the third day.
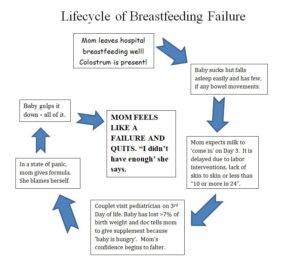
This was then followed by the beleaguered mother having a bout of doubt about her milk supply, supplementing with a bottle of formula (suggested, prescribed or even demanded by the care provider) and potentially quitting breastfeeding before her milk even had a chance to ‘come in’! Feeling dejected, she told herself “My body let me down and I didn’t have enough”.
When I teach about the impact of labor interventions and their possible effect on early latching, delayed onset of transitional milk and infant weight loss and gain in our Breastfeeding with Success class, I often see the light bulb moment for the 2nd time mothers who are attending because they were unsuccessful the first time. Suddenly they realize that they weren’t doing anything wrong, their body hadn’t failed and that the labor interventions were probably the initial cause of the problem. They also learn ways to counter obstacles caused by the labor (should they occur) and an overview of newborn weight gain (or loss) goals. My hope is that women leave the class armed and ready to try or try again. Knowledge is power.
One of the first topics we discuss is the effect of various medications and procedures during the labor – starting with Pitocin. Last year I began showing this video clip which summarizes a study (Brimdyr et al, 2015) of the effects of labor medications on latching and the nine newborn behaviors associated with the golden hour: Important Findings Published about Common Labor Medications and Breastfeeding Success – YouTube. The average baby does not latch for roughly 45 minutes but most have expectations of the baby latching within the first few. The Golden Hour should really be called the Golden Hours.
Pitocin is the Pits for Breastfeeding
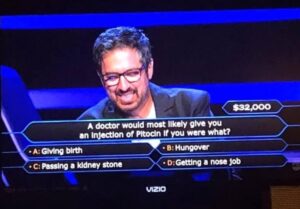
Of all the common drugs used during labor, Pitocin is probably the one that gives researchers the most cause for concern for breastfeeding because its use is associated with reduced APGAR scores, reduced newborn sucking in the first two hours (probably due to the negative impact on six cranial nerves from stronger contractions), higher likelihood of jaundice and delayed onset of milk production (aka milk coming in). With induction quoted at anywhere between 25%-50%, we must expect breastfeeding issues to be on the rise.
Use of Narcotics in Labor
More than 75% of women will request pain medication in labor – usually either a narcotic (like Nubain, Stadol, Fentanyl or Demerol) or more likely an epidural (containing Fentanyl). Pain medication in labor can be a positive choice for many reasons but studies suggest some medications used for pain management can be another hurdle to successful breastfeeding and that the longer the woman has been under the influence of the pain medication, the greater the potential impact.
Manufacturer’s guidelines warn that women who use narcotics should not breastfeed for four hours after receiving them. This is usually not a problem since narcotics are rarely given after 4cm dilation and labor usually has at least four hours left to go at that point. However if labor moved quickly and the baby was born with narcotics in his/her system, one could expect breathing problems, decreased alertness, a weak suck or a poor latch. In addition, the mother could encounter delayed onset of milk coming in.
Worry About the Fluid Load – Not the Epidural
While the fentanyl in an epidural can inhibit the nine newborn behaviors and ability to latch in the first 60 minutes of life (Brimdyr, K et al. 2015), the main hurdle to successful breastfeeding after an epidural seems to be fluid overload. A woman who requests an epidural will have a mandatory 1000 mL IV of Ringer’s Lactate to help maintain her blood pressure (which occasionally drops with an epidural), keep her hydrated and keep her labor progressing. After the epidural, the mother will continue to receive roughly 125mL of fluid every hour thereafter and will usually be denied drinking ‘by mouth’.
Fluid overload occurs when her fluids intake reaches 2500+ mL – which would be at the 13 hour mark (1000mL +125mL per hour) – or sooner if she had an IV for fluids as soon as she was admitted and an epidural. Water retention is acute because the mother’s body releases the excess over the next 24-48 hours after birth through urination. However a large fluid load can cause several distinct breastfeeding issues. A large fluid load can thin out colostrum, reduce or negate engorgement and delay transitional milk replacing colostrum for several days –resulting in a very hungry baby who may lose a lot of weight in the first 72 hours and need supplementing with formula. In some cases, women who take on >2500 mL of fluid during labor suffer from third spacing fluid retention. This is when excess fluid gathers in anything that hangs down (i.e. the breast) and can temporarily cause inverted nipples that make latching a newborn particularly difficult.
What Can We Do to Counter the Effects of Labor Interventions?
The first line of defense is my mantra: “Skin to skin to bring milk in”. Continuous skin to skin time with the baby in the first three days and encouraging the baby to feed from both breasts at each feed often really does help the move from colostrum to transitional milk. In class I advocate feeding the baby at least 8 times in the first 24 hours from both breasts at each session and then “10 or more in 24” until the baby is consistently gaining weight. It is also paramount that new mothers don’t rely on waiting for a baby to wake them for a feed – especially in those first 24 hours when babies are so sleepy. When I talk to women who are upset about weight loss and supplementing on Day 3, they almost always fed less than 8 times in the first 24 hours.
When the baby suddenly becomes ravenous on day 2, the mother can easily doubt her supply. “All the baby wants to do is feed!” she says. My lactation instructor used to compare intensely long periods of sucking on day 2-3 as ‘putting in an order at a restaurant’ and then waiting a day or two for it to arrive. I call that period of cluster feeding the ‘all you can eat buffet at the breastaurant’. It seems to make mothers remember the normalcy of the situation.
Another wise way to combat milk coming in slowly is to encourage the mother to hand express or hand pump colostrum several times a day in the first 48 hours – especially if the baby cannot be woken for a feed. Women who hand express in the first hour boost supply by up to 130% by week 6 (Parker, 2012). It can be stored and fed to the baby with a dropper or syringe. Hand expression can be a daunting concept so I’ve now started to show the first few minutes of Stanford School of Medicine’s video by Dr Jane Morton to normalize it: Hand Expressing Milk | Newborn Nursery | Stanford Medicine
Finally, supplementing with a few ounces of artificial baby milk/formula or banked breastmilk may seem counterproductive to breastfeeding but if weight loss is severe, it can solve the immediate problem while the mother’s body equalizes. Although there are downsides to early formula, it can often save the breastfeeding relationship instead of destroying it by taking the pressure off. There are no studies I can find (yet) that show any short or long term harm from supplementing with formula for 24-48 hours. However the mother should always feed the baby from her own body first.
Women should also be educated in recognizing the difference between breasts engorged with milk versus a breast swollen with fluids. A waterlogged breast often inverts the nipple and feels similar to the fleshy part of your arm. An engorged breast has firmness comparable to your wrist. Also, a woman who has had a large fluid load may not engorge (overproduce) with milk at all. If a woman is trying to latch a baby onto a breast swollen with excess fluids, urge her to try a technique called Reverse Pressure Softening. It is similar to making a sandwich with the breast but sandwiches the areola instead to evert the nipple so it protrudes out of the areola before latching.
Have you struggled to breastfeed or quit in the early days because of well-intended labor interventions? In the second part of the series, we will discuss newborn procedures that could skew weight loss, pediatric goals for newborn weight gain and look at a tool for determining if weight loss really falls into the supplementation zone.
References:
Abdoulahi M, Hemati Z, Mousavi Asl FS, Delaram M, Namnabati M. Association of Using Oxytocin during Labor and Breastfeeding Behaviors of Infants within Two Hours after Birth. Iranian Journal of Neonatology. 2017 Sep: 8(3).
Brimdyr, K et al. The Association Between Common Labor Drugs and Suckling When Skin-to-Skin During the First Hour After Birth. Birth 2015 42(4).
Healthy Children Project Inc. – Center For Breastfeeding. The Association Between Common Labor Drugs and Suckling When Skin-to-Skin During the First Hour After Birth – Healthy Children Project, Inc. (centerforbreastfeeding.org). Accessed 2.15.21.
Lind JN, Perrine CG, Li R. Relationship between use of labor pain medications and delayed onset of lactation. J Hum Lact. 2014;30(2):167–173.
Parker LA, Sullivan S, Krueger C, Kelechi T, Mueller M. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012.32(3):205-9.
About Mindy Cockeram
 Mindy Cockeram is a guest contributor for Connecting the Dots and a LCCE since 2011. She initially trained with the United Kingdom’s National Childbirth Trust (NCT), teaching both private classes and for the National Health Service at St Georges Hospital, London from 2004. Graduating from Villanova University in 1986, she earned a bachelor’s degree in Communications and a minor in Business Studies. Currently, she teaches childbirth and breastfeeding for a large non-profit hospital in Southern California. She released Cut Your Labor in Half: 19 Secrets to a Faster & Easier Birth in 2017. Two years later, she published Breastfeeding Doesn’t Have to Suck: Tips, Tricks and Knowledge for a Great Experience. She is currently writing her third book Pregnant Again? A Refresher for Childbirth & Breastfeeding due out in summer 2021.
Mindy Cockeram is a guest contributor for Connecting the Dots and a LCCE since 2011. She initially trained with the United Kingdom’s National Childbirth Trust (NCT), teaching both private classes and for the National Health Service at St Georges Hospital, London from 2004. Graduating from Villanova University in 1986, she earned a bachelor’s degree in Communications and a minor in Business Studies. Currently, she teaches childbirth and breastfeeding for a large non-profit hospital in Southern California. She released Cut Your Labor in Half: 19 Secrets to a Faster & Easier Birth in 2017. Two years later, she published Breastfeeding Doesn’t Have to Suck: Tips, Tricks and Knowledge for a Great Experience. She is currently writing her third book Pregnant Again? A Refresher for Childbirth & Breastfeeding due out in summer 2021.
Click to explore


Sorry, comments are closed for this post.